Healthcare Fraud
Healthcare fraud is the misstatement of facts – either knowingly or through unreasonable ignorance – that leads to unfair profit through medical coverage. Healthcare fraud encompasses false claims by physicians, managed care organizations, and numerous others. It also includes overpricing or incorrect invoices from manufacturers and distributors of such products as pharmaceuticals and wheelchairs. Healthcare fraud can even include individuals, such as those who attempt to gain coverage through identity theft.
Types of Healthcare Fraud
Healthcare fraud can occur on numerous levels. There are many ways in which a claim may be falsified, and various institutions that may be responsible. The following is a collection of the some of the most common methods of executing healthcare fraud.
Misstatement of Services
Perhaps the most common form of healthcare fraud is the misstatement of services rendered or goods provided. The goods/services may never have been given; some blatant scams set up shop with the specific purpose of obtaining insurance information and filing claims for fictitious medical treatment. However, many organizations have been known to engage in the subtler practice of “upcoding,” in which a claim contains a more expensive product or service than the actual one. This occurs in private practice, for example, when a doctor claims to have investigated symptoms of pneumonia in a patient that was never tested for anything more than a common cold.
Unreasonable Rates
Healthcare organizations are also infamous for charging unreasonable rates. Several high profile cases of government fraud have included healthcare equipment distributors that acquired their goods for pennies, then redistributed them at a cost of tens of dollars apiece to the government. But, just as with charging for services not rendered, there are less obvious ways of getting away with high rates. Physicians and other providers sometimes resort to a technique called “unbundling.” Unbundling involves splitting up the charges for a comprehensive procedure for which one all-encompassing charge is the industry standard. Each individual procedure can then be marked up without drawing as much attention.
Unnecessary Treatment
Third, some healthcare providers have been known to provide treatment that is completely unnecessary. This most often occurs in instances such as the pneumonia example, with the difference being that the attending physician actually performs the check even though the symptoms do not call for it.
Personal Expenses
Some providers have even combined personal expenses with their claims for medical care.
Kickbacks
Bribery, an illegal incentive given for the performance of a service – is not infrequent in the healthcare industry. Benefits agents may recommend one company’s plan over another’s in exchange for money. Or, in the course of care, an attending physician may recommend special treatment from one of his fellow providers over another with the knowledge that he’ll be paid for such a referral.
Consumer Healthcare Fraud
Consumers can also be guilty of healthcare fraud. One example is forging family names to provide coverage to friends. Consumers have also been known to encourage their provider in the forgery of claims with the intention of dividing up the reimbursement.
Prevention of Healthcare Fraud
Government agencies are constantly taking steps to try to combat healthcare fraud. Meanwhile, there are several things that individuals can do to protect themselves and help fight corruption.
Healthcare plan members should apprise themselves of their benefits and investigate bills and forms. It is important for consumers to protect their insurance cards and policy numbers. A person that allows disreputable healthcare providers access to this information is all but asking to have false claims filed in his or her name. (Incidentally, this is not just troublesome to the healthcare system; claims of false injuries or care can also plague a person’s medical records for years.)
Individuals should also be sure to investigate offers for free medical care, such as that offered in the context of a clinical study. These offers can sometimes form a front for illegal fraud schemes.
Finally, consumers can best fight fraud by reporting suspected cases.
The Federal False Claims Act
The Federal False Claims Act – or qui tam law – is a federal statute that allows citizens to file suits on behalf of the government against anyone who may be defrauding the state through a contractual agreement. The person who originally files the suit – called the relator – is given a portion of any damages the government receives. Most qui tam cases are filed against the defense and healthcare industries.
The False Claims Act was amended in 1986. Among the amendments were the inclusion of reckless disregard for procedure as a basis for a suit; applying the ‘preponderance of evidence’ clause that is used in most suits (previous false claims standards for evidence had been higher); an increase in the relator’s portion of the damages and an expansion of his or her responsibilities in completing the suit; and protection for relators. These provisions emboldened citizens, resulting in an increase in qui tam suits in the late 1980s and throughout the 1990s.
Contact an Attorney
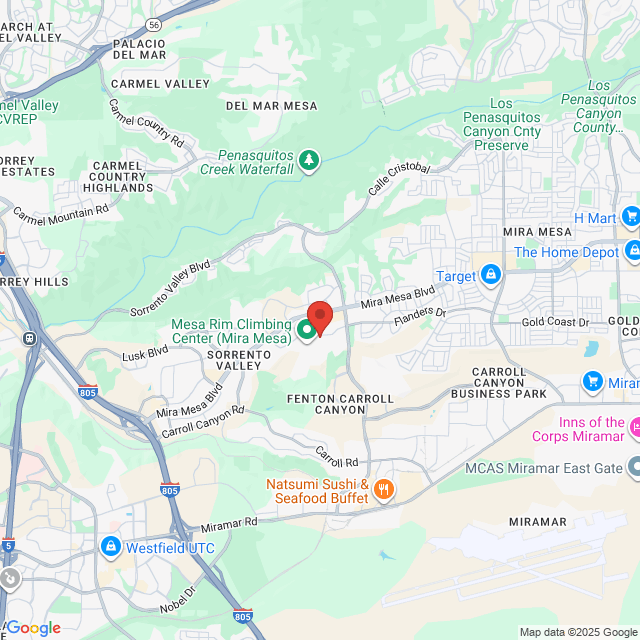
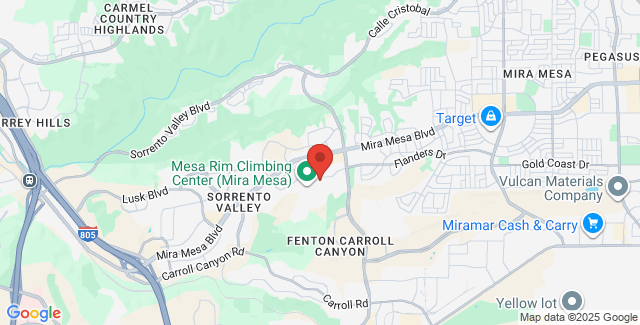
Please contact Impact Law to schedule a consultation with an attorney in your area to learn more about your legal options.